Joint hypermobility, often discovered when clinicians evaluate kids for another lower extremity issue, can cause pain, fatigue, and other symptoms that lead children to avoid exercise and drop out of sports. Hypermobile joints can also increase risk for traumatic injuries and for adult musculoskeletal conditions such as osteoarthritis.
Joint hypermobility, often discovered when clinicians evaluate kids for another lower extremity issue, can cause pain, fatigue, and other symptoms that lead children to avoid exercise and drop out of sports. Hypermobile joints can also increase risk for traumatic injuries and for adult musculoskeletal conditions such as osteoarthritis.
By Keith Loria
Joint hypermobility in children presents with ligamentous or capsular looseness and increased joint range of motion, which can lead to altered gait strategies and reduced dynamic balance. It’s linked to joint pain (the knee is commonly affected), and research suggests it’s a risk factor for musculoskeletal complaints, including the development of osteoarthritis later in life, and with knee joint and other injuries,1-3 particularly during contact sports.4
Joint hypermobility has been viewed as a mostly benign childhood disorder, but clinicians have now broadened this view to consider possible multisystem implications; joint hypermobility, for example, sometimes overlaps with Down syndrome, forms of Ehlers-Danlos syndrome, Marfan syndrome, and other disorders.5-7
Dawn M. Wahezi MD, MS, chief of the Division of Pediatric Rheumatology at the Children’s Hospital at Montefiore and associate professor at Albert Einstein College of Medicine, Bronx, NY, said joint hypermobility is thought to be “benign” when it is not associated with a hereditary disorder of connective tissue (eg, Marfan syndrome, Ehlers Danlos syndrome, or Stickler syndrome).
She noted that despite the relatively uncomplicated nature of benign joint hypermobility, the syndrome may lie along a broad clinical spectrum. It’s most often diagnosed (which is typically done with a series of positive mobility tests) when children present with symptoms that include joint pain, fatigue, gait abnormalities, and deformities such as flat feet.8
Oliver Fawcett, BPod, a podiatrist and founder of Foot Health Clinic 4 Kids in Samford, Australia, noted that in children with joint hypermobility the arches may sag, and the feet may roll in excessively because the strong ligaments that normally support the arch are overly stretchy and unsupportive, allowing the arches to collapse under the child’s weight.
The prevalence of benign, or generalized, joint hypermobility, has been reported to range from 2% to 57%, depending on age, sex, ethnicity, and the criteria used.9 Some studies have found a high prevalence of joint hypermobility in children and adults who practice specific sports, such as ballet10 and gymnastics.11
Diagnosis is often delayed.9 The average age of symptom onset is 6.2 years, but the average age at diagnosis is 9 years.12 Younger children tend to report more pain, which often lessens as children age and muscles and joints become tighter and stronger.
“Patients typically present with functional joint complaints that are episodic and self-limited,” Wahezi said. “In other cases, parents will report the child as being clumsy or poorly coordinated. Rarely, joint hypermobility can be associated with chronic pain syndromes and chronic fatigue syndrome.”
Kathy Martin, PT, DHSc, professor and assistant DPT program director at the Krannert School of Physical Therapy at the University of Indianapolis in Indiana, said the disorder can lead to developmental delay because the child has to work harder and develop greater strength to find the stability to achieve gross motor milestones like crawling, standing, and walking. Therefore, she said, she doesn’t classify it as a benign condition.
Joint hypermobility in children is a predictor of future joint pain. Children aged 10 years with hypermobility and musculoskeletal pain have an increased risk of pain persistence and recurrence in adolescence,13,14 and a 2014 study found children with joint hypermobility and without current joint pain had three times higher risk of developing joint pain in adolescence, though the association did not reach statistical significance.3
“Although children may not have pain, they likely will have significant pain and dysfunction as adults as a result of the joint hypermobility and abnormal wear and tear on their joints,” Martin said.
Parents are often anxious about their child with joint hypermobility, who may complain of general tiredness, fatigue, leg cramps, and its long-term impact, said Paul McDermott, PT, pediatric physiotherapy supervisor at Sidra Medicine in Doha, Qatar.
Pain, which is often starts during or after activity, is the predominant complaint of joint hypermobility, and can sideline kids from exercise and put them at risk for obesity. He noted symptoms of joint hypermobility are often shared among parents and siblings, and research suggests a strong hereditary component.15
 Musculoskeletal complications
Musculoskeletal complications
Children with generalized joint hypermobility need a higher degree of muscle stabilization during movement due to the looseness of their joints, explained Bente R. Jensen, PhD, associate professor in the Department of Exercise and Sport Science at the University of Copenhagen in Denmark. Jensen and colleagues recently conducted a study16 to examine muscle activation patterns of the knee muscles in girls aged 14 to 15 years with generalized joint hypermobility.
The Danish investigators recruited the girls randomly from a cohort of schoolchildren and hypermobility was assessed mobility with the Beighton score (range 0-9, with scores of greater than or equal to 6 indicating hypermobility), commonly used to diagnose joint hypermobility.
Participants performed isometric knee flexion and extension contractions with their dominant leg in a sitting position with the thigh horizontal.
A main finding was that girls with joint hypermobility had a 53% faster capacity for early rapid torque generation during knee flexion than girls without hypermobility despite no group differences in muscle strength. “This may reflect a motor adaptation to compensate for hypermobility,” said Jensen.
Girls with joint hypermobility also had higher medial-lateral co-contraction ratios during submaximal isometric contractions of the knee muscles compared with controls.16 “The medial side of the knee is the most common side for osteoarthrosis. The increased medial muscle activation in generalized joint hypermobility could play a role for the increased risk of osteoarthrosis later in life,” she said.
Moreover, girls with joint hypermobility had a reduced activation of their hamstrings during knee flexion compared with healthy controls,16 which Jensen said may contribute to excessive loading of the knee joint and increase the risk of injury.
The results are similar to those from an earlier study by Jensen and colleagues that included adults and children.17 In the adults with joint hypermobility, in whom joint pain is common, the researchers observed a reduced ability to control muscle force, which may be a result of their long-term hypermobility. Reduced control of muscle force is also seen in persons with osteoarthritis, Jensen said.
“Persons with joint hypermobility have muscle activation strategies of their knee muscles that are different from healthy controls,” Jensen said. “Their muscle activation strategy seems to increase the mechanical loading of their knees and will probably increase the risk of future knee problems.”
Management
The first principle in management of joint hypermobility, Wahezi said, is assessment for clinical manifestations suggestive of an inherited connective tissue disorder. Nonmusculoskeletal symptoms such as skin hyperelasticity, excessive bleeding or bruising, prominent veins, or heart murmurs should raise suspicion for potentially serious conditions such as Ehlers-Danlos syndrome, osteogenesis imperfecta, Marfan syndrome, and Larsen syndrome.18
“Reassurance and patient education are essential to ease any parental distress that may be associated with joint complaints,” she said.
Physical therapy. “Physical therapy is a key component in the management of symptomatic patients and should focus on muscle strengthening exercises and restoration of normal daily activities,” Wahezi said.
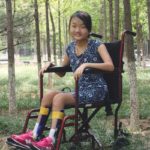
Martin suggests a protocol of strengthening in good alignment, weightbearing exercises to promote co-contraction, and, when indicated, compensatory strategies such as bracing and adaptive equipment. “Interventions should be individualized to the child’s needs, and there is no protocol or standard set of recommendations. In general, it might include standers, walkers, or even a wheelchair for long distances,” she said.
Jensen added that physical therapists should try to normalize a patient’s muscle activation pattern. This can be done by stimulating fast muscle force development through exercises from no force to a submaximal force level (eg, 50%-70% of maximum force).
“Additionally, physical therapists need to teach the patients how to move around without placing high loads on their knees [eg, keeping knees directly over the feet during knee flexion, avoiding twisting in the knees, and avoiding hard impacts],” she said.
Orthoses. Foot orthoses are sometimes prescribed to patients with joint hypermobility, with the goal of stabilizing their gait pattern and theoretically reducing the associated fatigue and joint pain. However, research on the efficacy of orthotic interventions is sparse.
The appropriateness of orthotic intervention depends on many individual factors, said Martin.
 Pain that limits function is a potential indication for orthoses. The practitioner must evaluate how the joint hypermobility affects movement and functional activities, and then decide if an orthosis might optimize function and promote more normal movement, she said.
Pain that limits function is a potential indication for orthoses. The practitioner must evaluate how the joint hypermobility affects movement and functional activities, and then decide if an orthosis might optimize function and promote more normal movement, she said.
“There really is no ‘one size fits all’ solution to this—no algorithm that identifies who gets orthoses and who doesn’t,” Martin said. “When deciding what type of orthosis is best, it really depends on what the movement dysfunction is and what the goal of intervention is.”
She prefers to go with the least restrictive device and the most dynamic material (thinner, more flexible plastic) that will allow as close to normal movement as possible and would use a rigid device only to prevent motion to help relieve pain or protect a joint from further damage.
Long-term splinting may lead to weaker muscles and further deconditioning and thus should be avoided, though Wahezi noted short-term use may be helpful. Stabilizing footwear with medial post support may also be helpful in children with pes planus and joint hypermobility.19
Often patients do not require customized insoles, given the predominantly normal foot shape of most kids with generalized joint hypermobility, said McDermott. Insoles that work best, in his opinion, offer a deep heel cup and reactive/dynamic arch support.
“The principle behind using the heel cup is to provide stability and improve control of gait. In our clinic, it was generally felt that insoles improved the walking pattern and control of children with joint hypermobility, but this was previously based on our observation only,” he said.
He and colleagues set out to test their observations in a study20 that was published in February in Gait & Posture. “Our aim was to investigate our hypothesis in a small pilot study group using an electronic sensor mat that measures and records temporospatial patterns of the gait cycle.”
McDermott and colleagues recruited 21 patients (13 girls; median age, 10 years) and analyzed their gait while they walked in their own footwear and immediately after applying full-length over-the-counter insoles, which had deep heel cups, high medial borders, and heat-moldable shells. The investigators tested children as they walked on the mat at their preferred speed and after being asked to walk more slowly.
Children demonstrated a significant reduction in step length and width variability with the orthoses.19 “The insoles had an immediate, positive effect on gait, which became more synchronized,” McDermott said.
“My personal view [on management] is to carry out a thorough assessment of the child’s joints, muscle strength and endurance, and pain score,” he said. “I also consider the parents’ view on pain levels and general function levels.”
His treatment program for most kids includes one or more of the following: modification of activity (not complete rest, he advises, as it’s important that muscles stay conditioned to support joints); advice to wear footwear with a stable heel counter at least 60% of week; prescription of an off-the-shelf orthosis that promotes heel stability during stance phase; and a strengthening program focusing on antigravity muscle groups.
He first improves footwear that is used for both daily walking and high-impact activity. For patients who have poor heel push-off in supported single-leg stance coupled with flexible pes planus, he encourages the use of a flexible, stabilizing generic insole.

These over-the-counter insoles used in a 2018 Gait & Posture study had an immediate positive effect on gait in children with joint hypermobility, reducing step length and width variability. (Photo courtesy of PPL Biomechanics.)
Challenge of underdiagnosis
As noted, joint hypermobility is underdiagnosed. “Muscle fatigue or an unwillingness to walk in younger children are important indicators that shouldn’t be dismissed,” McDermott said.
“Parents often report that their child prefers to sit in a buggy or be lifted than walk independently. This can sometimes be dismissed as lazy or behavioral until a diagnosis of hypermobility is confirmed,” he said.
With older children or young adults, McDermott said practitioners should pay special attention to disinterest in physical activities or a refusal to participate in sports. Furthermore, discussions with young patients should include questioning that helps them articulate symptoms of fatigue, as describing pain alone may miss the point.
“Joint hypermobility continues to be under-recognized, as most patients remain asymptomatic,” Wahezi said. “That’s why careful physical examination and increased recognition is crucial to avoid unnecessary diagnostic testing and to institute appropriate management and prevent potential future complications.”
In her view, increased awareness among practitioners will increase patient and parent education, decrease potential anxiety, and expedite necessary interventions.
“With increasing knowledge of the potential impact joint hypermobility can have on quality of life, adequate education of families is essential to prepare them for potential future complications,” she said.
Keith Loria is a freelance writer in northern Virginia.
- Konopinski MD, Jones GJ, Johnson MI. The effect of hypermobility on the incidence of injuries in elite-level professional soccer players: a cohort study. Am J Sport Med. 2012;40(4):763-750.
- Tobias JH, Deere K, Palmer S, et al. Joint hypermobility is a risk factor for musculoskeletal pain during adolescence: findings of a prospective cohort study. Arthritis Rheum. 2013;65(4):1107-1115.
- Grahame R. The multisystemic nature and natural history of joint hypermobility syndrome and Ehlers–Danlos syndrome in children: New research data conflict with widely held views. Rheumatol 2017;56(12):2048-2049.
- Adib N, Grahame R, Woo P, Murray KJ. Joint hypermobility syndrome in childhood. A not so benign multisystem disorder? Rheumatology 2005;44(6):744-750.
- Quanbeck D, Greer K, Wilkins K. Joint hypermobility: normal variation or cause of concern? Gillette Children’s Specialty Healthcare: A Pediatric Perspective 2013;22(1):1-3.
- Cattalini M, Khubchandani R, Cimaz R. When flexibility is not necessarily a virtue: a review of hypermobility syndromes and chronic or recurrent musculoskeletal pain in children. Pediatr Rheumatol Online 2015;13:40
- El-Metwally A, Salminen JJ, Auvinen A, et al. Lower limb pain in a preadolescent population: prognosis and risk factors for chronicity–a prospective 1- and 4-year follow-up study. Pediatrics 2005;116(3):673-681.
- Hakim AJ, Cherkas LF, Grahame R, et al. The genetic epidemiology of joint hypermobility: a population study of female twins. Arthritis Rheum 2004;50:2640-2644.
- Jensen BR, Jesper S, Pia SM, et al. Alterations in neuromuscular function in girls with generalized joint hypermobility. BMC Musculoskelet Disord 2016;17:410.
- Jensen BR, Olesen AT, Pedersen MT, Kristensen JH, Remvig L, Simonsen EB, Juul-Kristensen B. Effect of generalized joint hypermobility on knee function and muscle activation in children and adults. Muscle Nerve 2013;48(5):762-769.
- Quanbeck D, Greer K, Wilkins K. Joint hypermobility: Normal variation or cause for concern? Pediatric Perspective 2013;22:1.
- Wahezi D, Ilowite N. Joint problems and hypermobility. Pediatrics Rev 2009;30;187.
- McDermott P, Wolfe E, Lowry C, et al. Evaluating the immediate effects of wearing foot orthotics in children with joint hypermobility syndrome (JHS) by analysis of temperospatial parameters of gait and dynamic balance: A preliminary study. Gait Posture 2018;60:61-64.