
The updated guidelines recommend that children meet daily physical activity goals through a wide variety of play and sport. (Images used courtesy of the US Department of Health and Human Services.)
The new federal physical activity guidelines include the first-ever recommendations for children aged 3 to 5 years, as well as updated guidelines for older kids. Here, we cover what you need to know about the new advice and offer tips from experts to help kids with lower extremity conditions get and stay active.
By Keith Loria
The US Department of Health and Human Services on November 12 unveiled a second edition of its physical activity guidelines1 (the first edition was published in 20082). Its message for pediatric lower extremity practitioners is that their care should facilitate as much physical activity (PA) as possible for young patients, including educating parents about why PA is so important and how they can help their kids reach activity goals.
Katrina L. Piercy, PhD, RD, ACSM-CEP, Department of Health and Human Services physical activity and nutrition advisor, said the guideline update is based on new evidence highlighting the importance of physical activity for health for individuals of all ages. It includes the first-ever federal recommendations for children aged 3 to 5 years as well as updated guidelines for youth aged 6 through 17 years. The 2008 guidelines included recommendations for kids aged 6 years and older, but Piercy said there’s now evidence to make recommendations for preschool-aged children.
“We realized there had been a huge growth in scientific evidence and felt like we needed to update our recommendations to the public and talk about the fact that most Americans aren’t meeting these guidelines,” she said. “This also gave us an opportunity develop a communications campaign to help get these messages out and reinforce why physical activity is important.”
The “Move Your Way” campaign based on the new recommendations is designed to help health professionals, national organizations, communities, and other physical activity stakeholders clearly communicate the amount and types of physical activity that Americans need to stay healthy—as well individualized strategies to help kids and adults meet those goals. Practitioners can access interactive tools, fact sheets, posters and other educational materials, including those designed for parents, at health.gov/paguidelines/moveyourway.
Piercy noted the key takeaway is that kids of all ages should be getting physical activity through a variety of activities.
Three hours a day for preschoolers

The “Move Your Way” website offers fact sheets and other education resources practitioners can share with parents.
“The new guidelines for children aged three through five emphasize that preschool-aged children should be active throughout the day to enhance growth and development,” she said. “Adults supervising children this age should encourage a variety of types of active play.”
Although the specific amount of activity needed to improve bone health and avoid excess fat in young children is not well defined, a reasonable target is three hours per day of activity of any intensity (light, moderate, or vigorous), according to the guidelines. This, the guidelines note, is the average amount of activity observed among children of this age and is consistent with guidelines from Canada, the UK, and Australia.
Physical activity for this age group should include unstructured “free” play, as well as activities such as throwing games and bicycle or tricycle riding. To strengthen bones, young children should do activities that involve hopping, skipping, jumping, and tumbling.
“The three hours the guidelines recommend for preschool children can vary in intensity and [the guidelines] are vague in the types of activity recommended,” said Carlos Uquillas, MD, a pediatric sports medicine specialist and pediatric orthopedic surgeon at Cedars-Sinai Kerlan-Jobe Institute in Los Angeles. “However, it is important to know what amount of activity is being performed at school and how much should be done at home. It is particularly important to ensure kids of this age are having enough physical activity, as they are undergoing such rapid growth both physically and emotionally.”
Moderate-to-vigorous PA for older kids
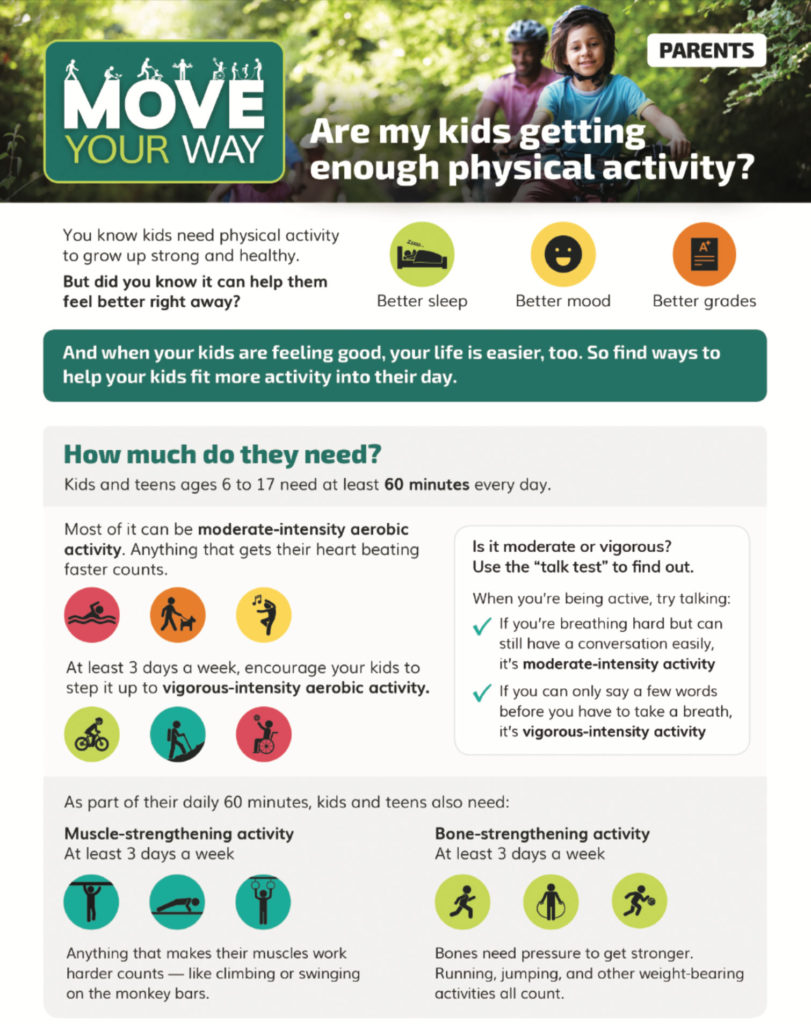
The “Move Your Way” campaign has many educational resources for parents, including this fact sheet on activity for children aged 6 to 17 years.
Children aged 6 years and older should get 60 minutes or more daily of a variety of mostly moderate- or vigorous-intensity PA (versus light activity) that’s enjoyable and appropriate for their age, the guidelines report. Piercy noted that, at least three days a week, the daily PA goal should be composed of mostly vigorous exercise because of the greater improvement in cardiorespiratory fitness intense workouts offer compared with light and moderate activity.
Evidence indicates that both acute bouts and regular moderate-to-vigorous physical activity improve the cognitive functions of memory, executive function, processing speed, attention, and academic performance of school-aged children, Piercy said.
The guidelines also advise that these children should include three days a week of both muscle-strengthening and bone-strengthening exercises as part of their daily PA goal. Bone-strengthening activities remain especially important for children and young adolescents because the greatest gains in bone mass occur during the years just before and during puberty and the majority of peak bone mass is obtained by the end of adolescence.
Per the new guidelines, any episode of moderate- or vigorous- intensity PA, however brief, counts toward the 60-minute daily recommendation, Piercy said. The 2008 guidelines for adults noted only 10-minute or longer exercise bouts counted toward daily requirements. Now all PA, however intermittent or short, counts toward daily totals for both kids and adults.
“Growing evidence demonstrates the immediate health benefits attainable from a single bout of activity, including reduced anxiety and blood pressure, improved quality of sleep and improved insulin sensitivity; therefore, those time limitations have been removed,” Piercy said. “We now emphasize that any amount of physical activity counts, and any type of movement can have positive benefits.”
Jennifer Laine, MD, a pediatric orthopedic surgeon at Gillette Children’s Specialty Healthcare-St. Paul in Minnesota, said the report shows that regular physical activity can improve health in multiple ways, including reducing gains in body weight and improving bone health, even in the younger age group.
“It is well-recognized that childhood obesity is a significant public health problem. Sedentary activities and lifestyle play a significant role in this,” she said. “The updated guideline shows that increased physical activity affects certain aspects of health—weight gain and bone health, for example—that can track into adult life. It supports building physical activity into multiple environments when possible.”
School programs can be effective, but it is helpful if activity can be worked into other realms, such as biking for transportation instead of motorized travel, she said.
PA for kids with disabilities
When possible, children and adolescents with disabilities should meet the key PA recommendations for their age group, the guidelines advise. The recommendations encourage as much physical activity as children’s individual abilities allow and note that when young people can’t participate in the appropriate types or amounts of PA needed to meet key guidelines, they should be as active as possible and avoid being inactive.
“Children and adolescents with disabilities are more likely to be inactive than those without disabilities. Youth with disabilities should work with a healthcare professional or physical activity specialist to understand the types and amounts of physical activity appropriate for them,” Piercy said.
At Gillette Children’s Specialty Healthcare, Laine works closely with the Department of Therapeutic Recreation to help kids and families find activities that suit them. (See “Therapeutic play plus O&P care is a win-win for kids,” November 2016, page 11.)
“There are nearly always ways to build physical activity into a child’s life, no matter what the condition,” she said. “What is important and essential is getting kids active early in life and involving them in activities that get them moving beyond what they do typically for their activities of daily living. This has different meanings for different children. It is important for children to try a variety of activities when they are young, and then they can pick what they like as they grow older.”
In addition to the overall health benefits of being physical active, giving children the opportunity and encouragement to participate in these activities has social benefits, as well, Laine said. “They can interact with other children, learn how to take turns, learn how to be a part of a team, learn sportsmanship, and even learn general social rules such as how to stand in line,” she said.
Physical and occupational therapy often plays a key role in maintaining activity levels for kids with disabilities, said Uquillas. “Kids with limited lower extremity function may be able to get significant physical activity and its benefits from upper extremity exercise. The benefits of activity go beyond the physical gains, but also include psychological, social, and developmental gains,” he said.
Below, Uquillas and others discuss ways to promote physical activity in kids with several specific lower extremity issues.
Injury
“In terms of people treating injuries, the guidelines didn’t look at specific interventions, but the biggest takeaway is to work with someone who knows how to tailor an activity and set the child on a positive path in doing that activity,” Piercy said.
Uquillas said that kids with lower extremity injuries face challenges in complying with the guidelines when they have weightbearing restrictions, have to elevate, or are limited due to assistive devices such as crutches. In many cases, he said, injuries are temporary, which can result in just a temporary decrease in activity. “In this case, after consultation with a doctor, kids should try to remain active without compromising their healing,” he said.
“In this age group, temporary injuries are typically fractures, and often are treated with immobilization and activity restrictions,” he said. “If it’s necessary to avoid weightbearing, it becomes more challenging to stay active. Water therapy or swimming can be a good activity in this scenario. Waterproof casts and braces can be used.”
In older children and adolescents, fractures continue to be a common injury; however, at this age sprains, strains, and overuse injuries also occur. Physical therapists and athletic trainers can help children rehabilitate from these injuries and safely return to active play and sports, he said.
Lev Kalika, DC, RMSK, clinical director of the New York Dynamic Neuromuscular Rehabilitation & Physical Therapy Clinic in New York City, noted that training the upper body while the lower body heals from injury helps maintain overall fitness.
Cerebral palsy
Adaptations can help kids with conditions like cerebral palsy (CP) participate in a wide variety of activities, said Jennifer Laine.
Even if kids with CP don’t use a wheelchair in daily life (instead using a walker, for example), she said, they might use a wheelchair might as a piece of sports equipment so they are able to play adaptive basketball.
“For some children who use a wheelchair for distances, they may walk with a walker as their physical activity for a certain amount of time each day,” she said.
Sara B. Rubinstein, CO, LO, TRS, an orthotist at the Ann & Robert H. Lurie Children’s Hospital of Chicago, said patients with CP often participate in power chair soccer or bocce competitions.
“Orthotics and a proper wheelchair seating system can provide a secure base for patients to drive their chairs through the games while weaving between players and performing spin kicks,” she said. “AFOs with leg straps can protect the lower limbs from potential injury while supporting the athlete while they play.”
Joint hypermobility
Patients with joint hypermobility and arthralgia can often benefit from custom foot orthoses and supportive footwear, said Rubinstein. “Presentations we see in these populations include hindfoot valgus, genu valgum, and knee hyperextension. The combination of custom foot orthoses and supportive footwear with a semirigid heel counter can resist the patient’s tendencies towards end-range positioning,” she said.
“Physical therapy can promote midrange strengthening and postural awareness to reduce the endpoint stress patients can put on their joints,” she added. “Low-impact exercise such as cycling, Pilates, and swimming are often a good fit for patients with hypermobility.”
Crawling-type movements engage the entire body and provide a challenging exercise when patients cannot load their feet, which can be an issue for children with joint hypermobility, said Kalika.
“Children with joint hypermobility have loading issues because they are usually hyperpronated and hyperextended in their knees; therefore, during gait the timing on knee flexion, hip flexion and foot pronation never couples into a shock-absorbing mechanism that is shared throughout all of these joints,” he said.
Flatfoot
Kamran Hamid, MD, a foot and ankle surgeon with Midwest Orthopaedics at Rush University Medical Center in Chicago, said in a majority of children, flatfeet are a completely normal finding and should not limit their physical activity.
“I encourage parents to purchase supportive shoes and encourage their children to participate in sports and activities with their peers,” he said. “Orthotics are not necessary in children with flatfeet unless their feet are painful. Children with painful flatfeet should see an orthopedic doctor specializing in pediatric orthopedics or foot and ankle orthopedics for evaluation and potential treatment with orthotics, physical therapy, or other modalities.”
Caleb Backe, ACSM-CEP, a certified personal trainer with Maple Holistics in Farmingdale, New Jersey, said a good technique for youth with flatfeet is to roll a tactile ball along the arch of the foot to activate the muscles; it should be done as a relaxing warmup before more strenuous activities.
He also recommends using a large therapy ball for children with more severe presentations. “Have the child stand on the ball while you hold their hands and encourage them to jump up and down,” Backe said. “This engages their feet and ankles fully, as well as working the rest of the body.”
Obesity
Obesity and associated physical ailments are on the rise in the US, and numerous studies3,4 have identified childhood as the beginning of many lifestyle factors that result in poor adult health.
“The updated federal activity guidelines reflect the need to ingrain salubrious activity choices in our children to prevent downstream health consequences such as obesity,” Sara Rubinstein said.
In some instances, children have already reached body mass index criteria for obesity prior to an intervention and are often embarrassed to participate in activities with their peers due to self-consciousness or potential bullying.
“Increased activity is sometimes not enough in these cases,” Hamid said. “There are adolescent/pediatric weight loss programs associated with health systems that may be available for nutrition counseling and exercise coaching for these kids.”
Additionally, patients with diseases such as muscular dystrophy or Charcot-Marie-Tooth disease will often report an increase in falls or more difficulty staying on their feet when they experience significant weight gain.
“It is part of our duty as healthcare professionals to educate our patients on the additional health concerns related to weight gain and support them to be as active as possible as this can directly affect their mobility down the road,” Rubinstein said. “Utilizing pediatric physiatry in multidisciplinary clinics is another great way to promote overall wellness with pediatric patients.”
Keith Loria is a freelance writer in northern Virginia
- Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report, 2018. Washington, DC: U.S. Department of Health and Human Services; 2018. https://health.gov/paguidelines/second-edition/report/. Published November 12, 2018. Accessed December 18, 2018.
- Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report, 2008. Washington, DC: U.S. Department of Health and Human Services; 2008. https://health.gov/paguidelines/2008/report/. Accessed December 18, 2018.
- Huh SY, Rifas-Shiman SL, Taveras EM, Oken E, Gillman MW. Timing of solid food introduction and risk of obesity in preschool-aged children. Pediatrics 2011;127:e544-551.
- Fiese BH, Bost KK, McBride BA, Donovan SM. Childhood obesity prevention from cell to society. Trends Endocrinol Metab 2013;24(8):375-377.





